More COPD patients than you may realise need3,9,21
Patient Profiles
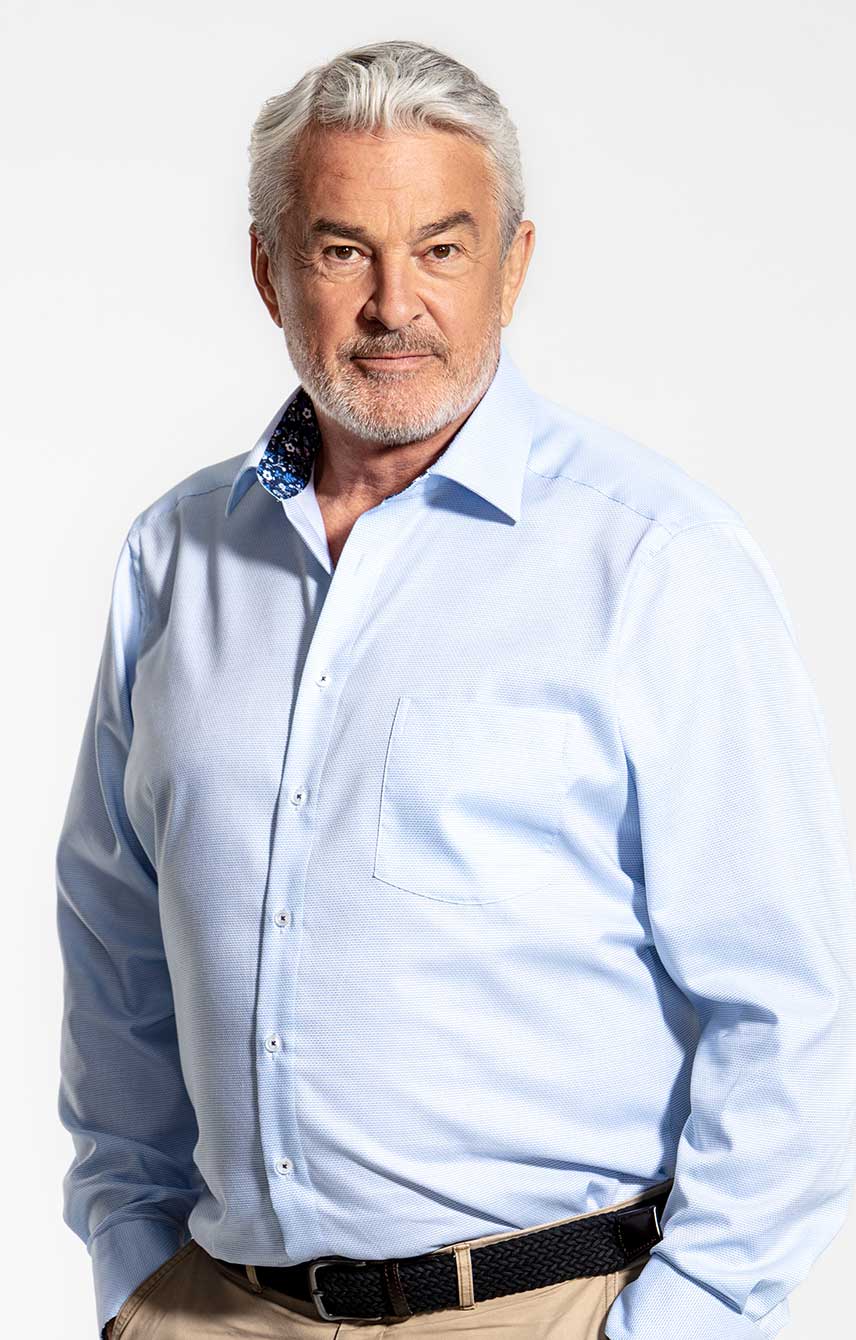
Bernard, 74 years old

Background
- Recently diagnosed with COPD
- Symptoms include severe breathlessness throughout the day, often keeping him awake during the night. He had a single exacerbation at diagnosis, which did not lead to hospitalisation
- Recently initiated on LAMA/LABA FDC delivered via a DPI, but he struggles to inhale from the device and his symptoms are not well controlled
- Bernard was found to have suboptimal peak inspiratory flow (sPIF)
Treatment considerations: initiation and next steps
-
Initiation with LAMA/LABA dual bronchodilation was the optimal choice for Bernard:
- LAMA/LABA offers superior symptom control over LAMA or LABA monotherapy1,2
- Inhaled corticosteroids are only recommended for a subset of patients, those with high exacerbation risk3,4 and high blood eosinophil count.3 Inhaled corticosteroids are not recommended for Bernard
- However, some DPIs require a forceful inhalation to optimally separate the medicine from carrier particles5-8
- Bernard has sPIF*, which may be associated with poor COPD outcomes9,10 as medication may not be delivered optimally5,6
- sPIF* is not uncommon; up to 52% of COPD patients struggle to inhale9
- Switch to SPIOLTO® RESPIMAT® for active delivery of LAMA/LABA via a soft mist inhaler, independent of Bernard's ability to inhale11-13
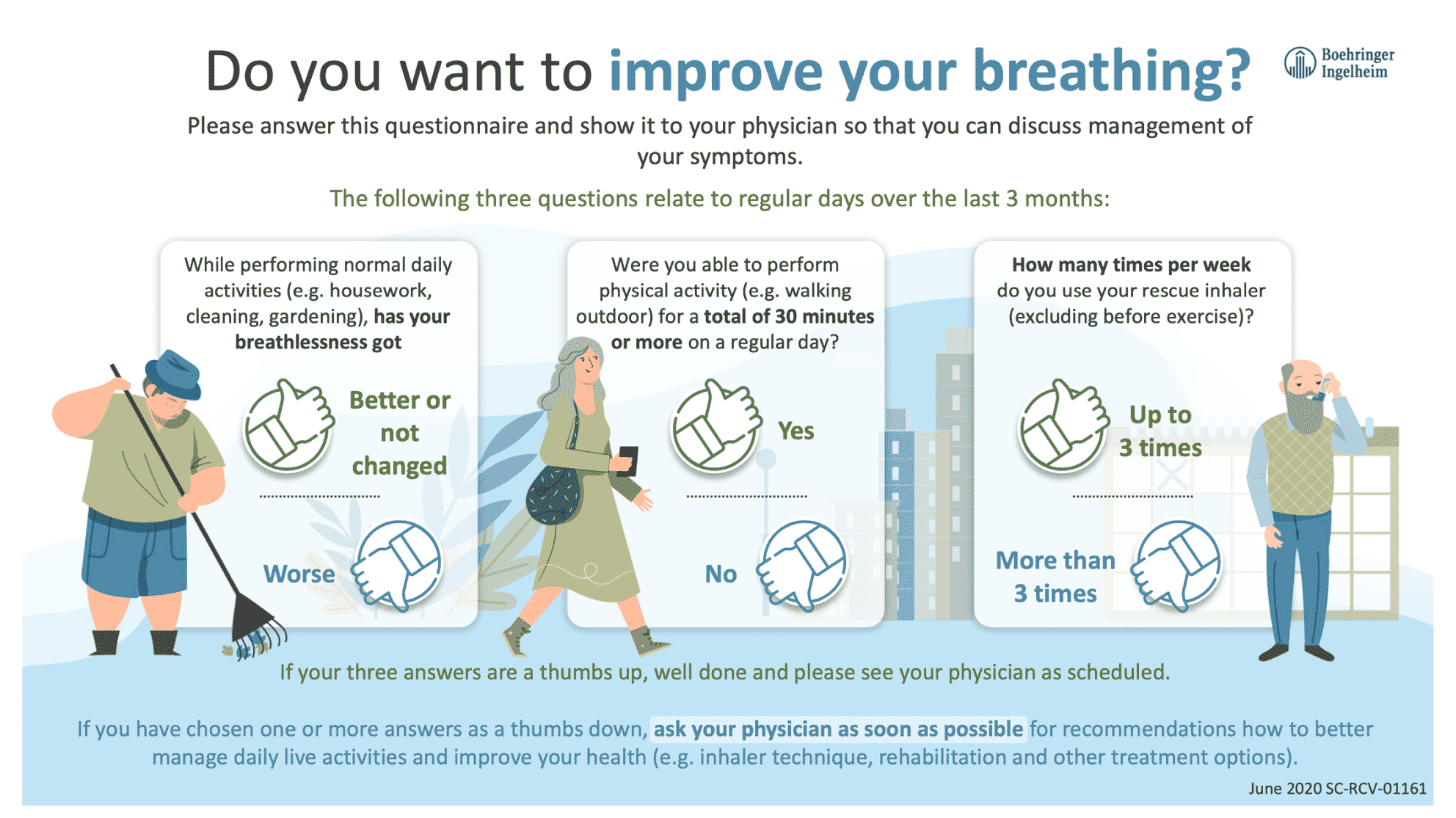
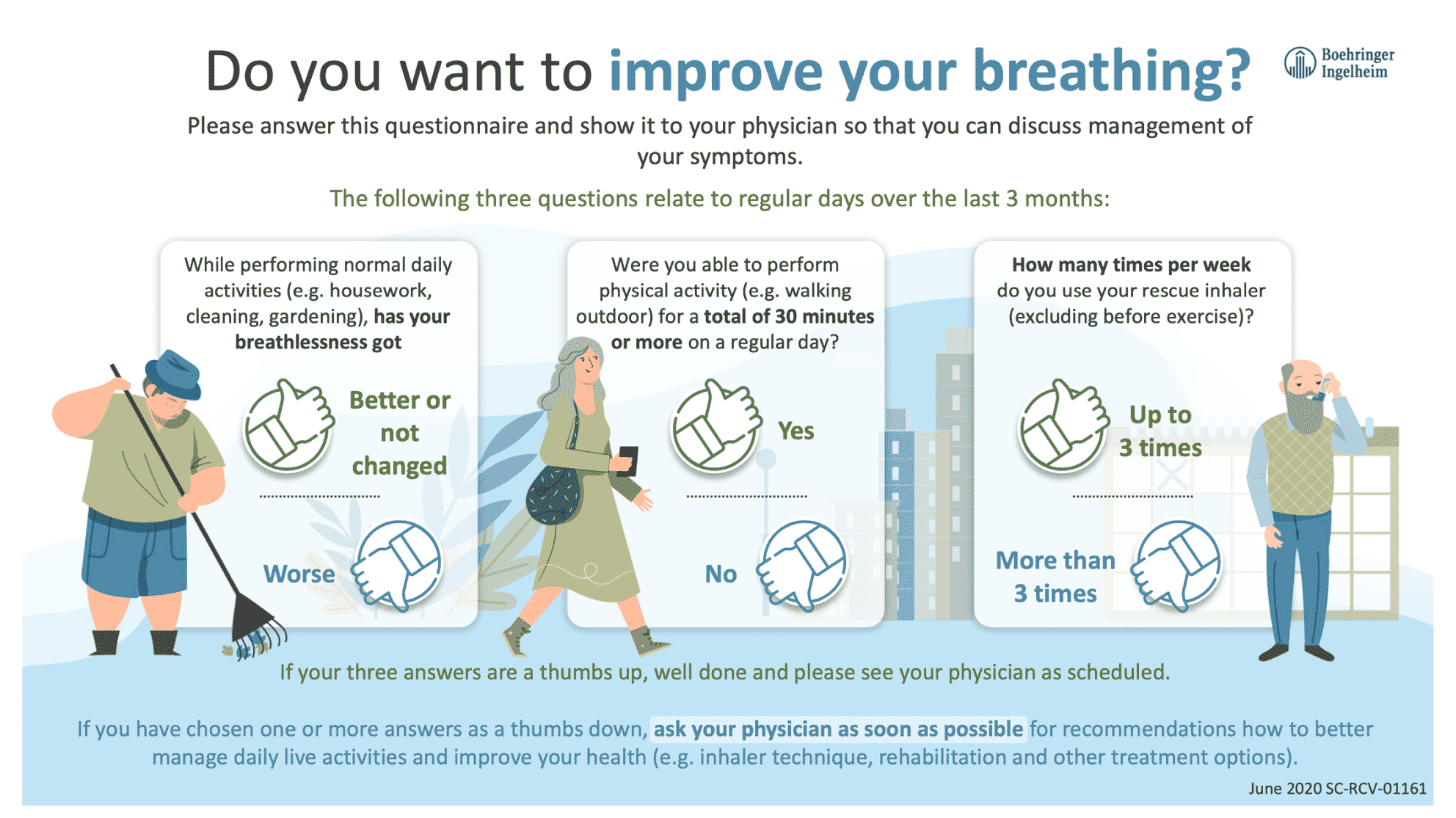
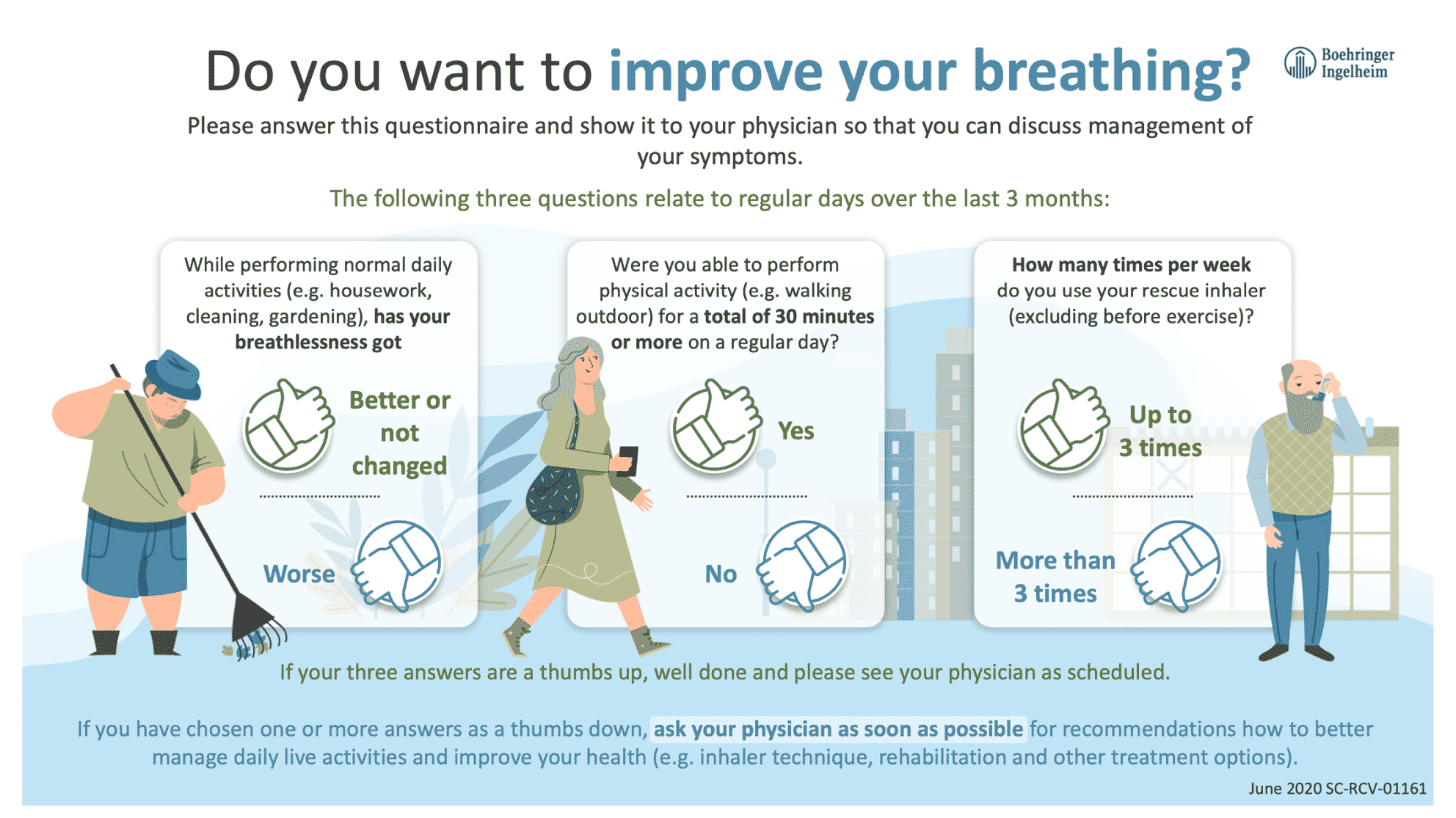
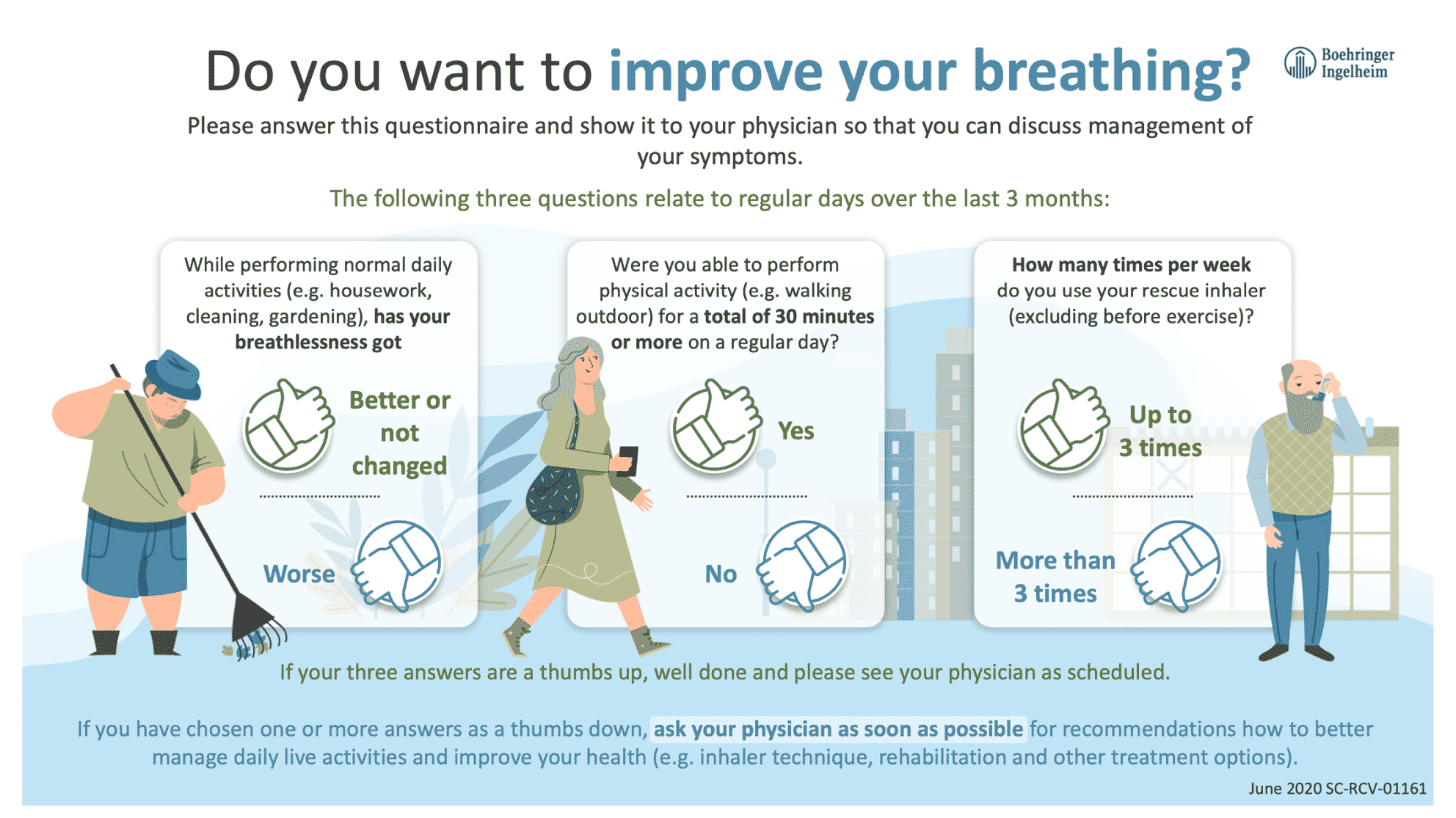
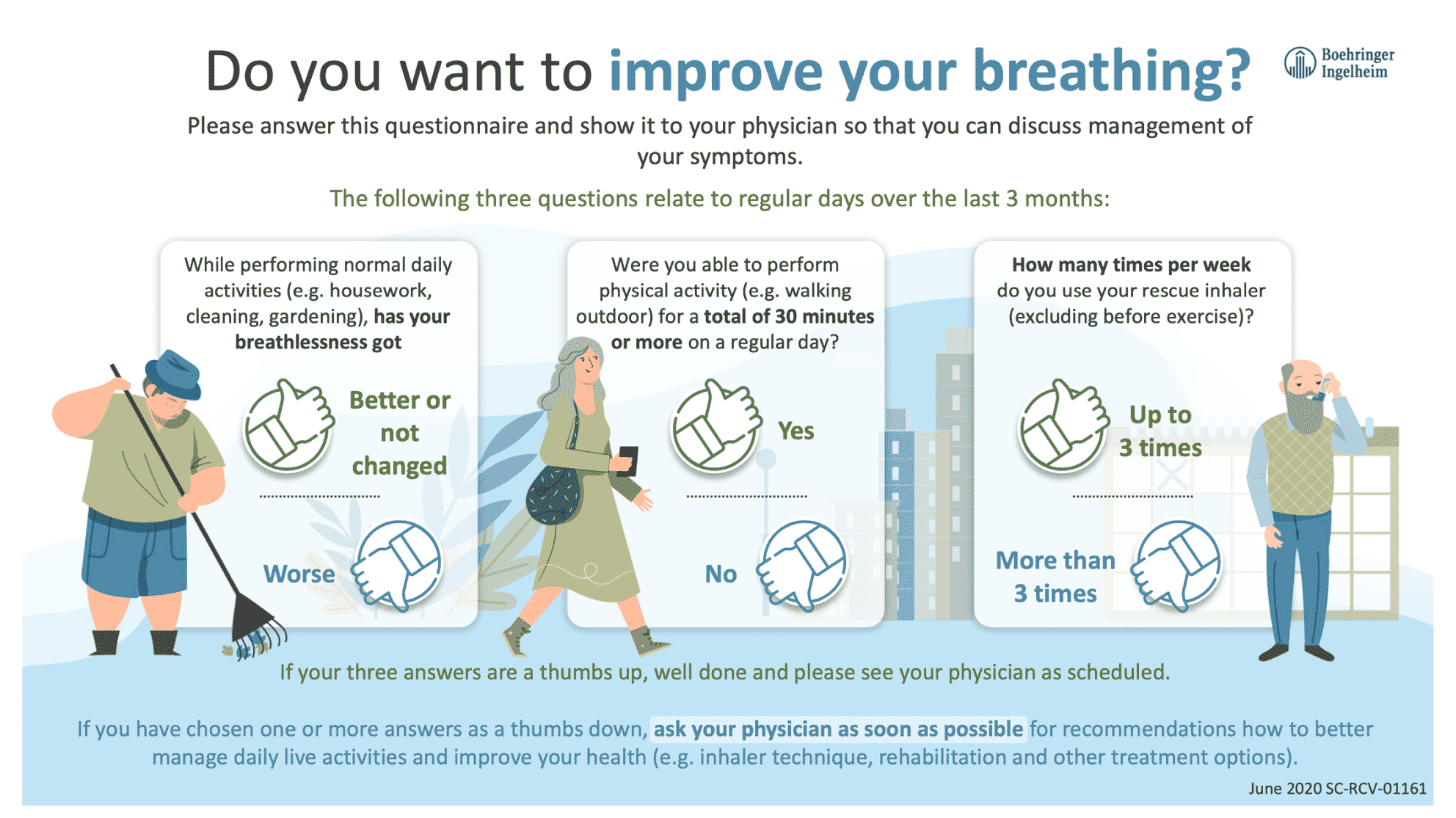
Dr. Miller's Simple Tools & Tips
- Infographics
- Content 1
- Inhalation Video
- Content 2
- Stand/Sit Exercise
-
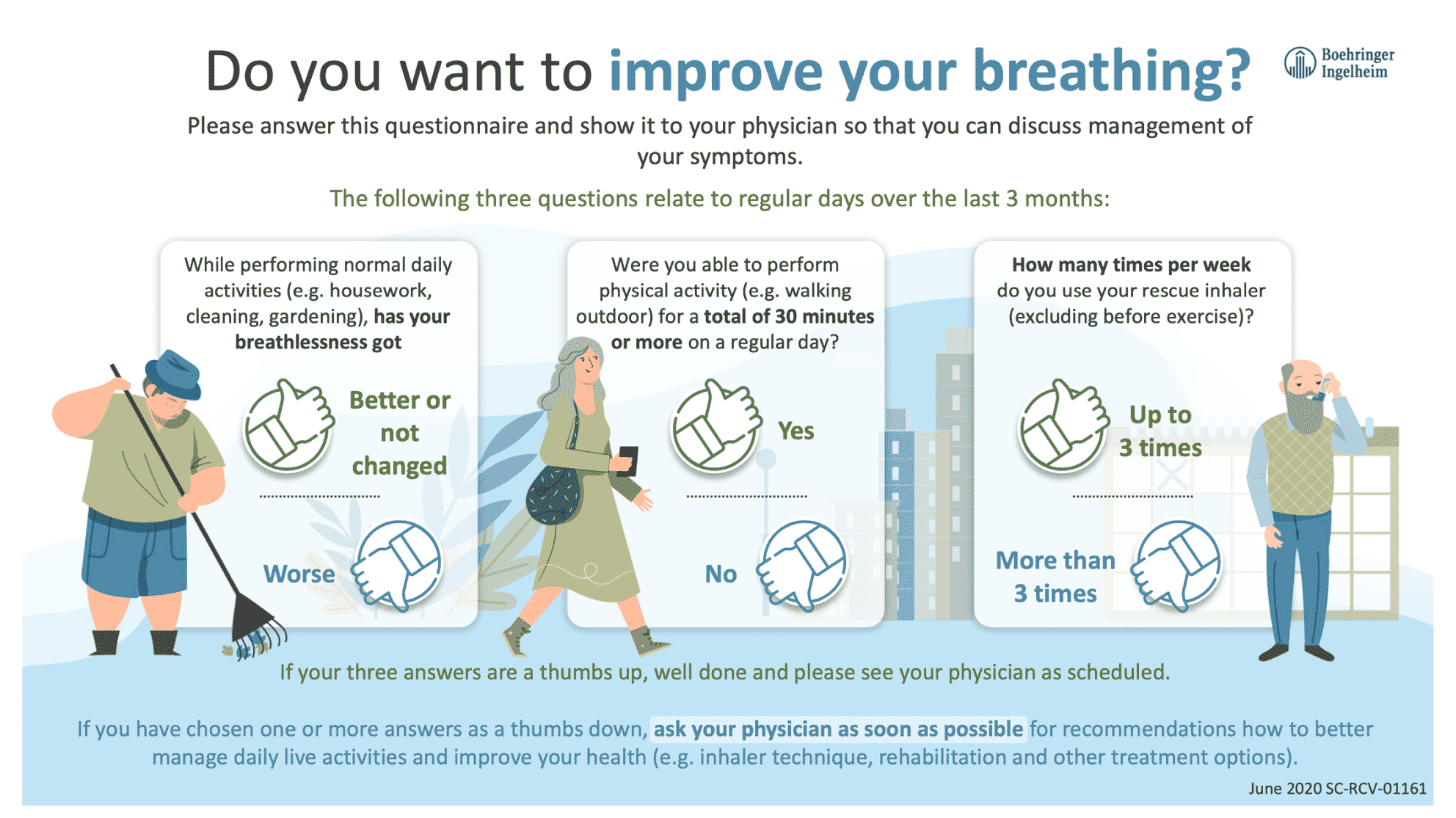
- Patient Questionnaire
-
Carolina, 61 years old
Background
- Diagnosed with COPD 6 months ago
- Carolina was very active before she was diagnosed with COPD, swimming and playing tennis regularly. This is now limited by her symptoms though, which include breathlessness on exertion. She does not have a history of exacerbations
- Her blood eosinophil count is 150 cells/μL
- She was initiated on LAMA/LABA delivered by an DPI at diagnosis, but she is still experiencing symptoms
Treatment considerations: initiation and next steps
-
LAMA/LABA initiation was the optimal choice for Carolina:
- LAMA/LABA offers superior symptom control over LAMA or LABA monotherapy1,2 for patients like Carolina
- Inhaled corticosteroids are only recommended for a subset of patients, those with high exacerbation risk3,4 and high blood eosinophil count.3 Inhaled corticosteroids are not recommended for Carolina
- However, up to 52% of COPD patients struggle to inhale from their device9 – meaning that the therapy is not delivered optimally.5,6 Carolina is receiving LAMA/LABA via a DPI
- Carolina is still symptomatic despite dual bronchodilation. Before escalation of therapy, GOLD recommends assessment of inhaler technique and adherence and the role of non-pharmacological approaches3
- GOLD recommends assessment of inhaler technique with retraining as required. Switching inhaler device may be appropriate3
- Switch to SPIOLTO® RESPIMAT® for active delivery of LAMA/LABA via a soft mist inhaler14
- SPIOLTO® RESPIMAT® improves activity-related breathlessness and exercise endurance time, which can help Carolina to resume her previously active lifestyle15,16

Dr. Miller's Simple Tools & Tips
- Infographics
- Content 1
- Inhalation Video
- Content 2
- Stand/Sit Exercise
-
- Patient Questionnaire
-
Stacy, 54 years old

Background
- Recently diagnosed with COPD
- Symptoms on presentation included severe breathlessness throughout the day, and she walks slower than friends of the same age. She does not have a history of exacerbations
- Stacy has only just been diagnosed and has not yet initiated maintenance therapy for COPD
Treatment considerations: initiation and next steps
- ATS 2020 guidelines recommend LAMA/LABA as a first-line treatment option in patients with dyspnoea or exercise intolerance4
- Stacy is experiencing severe breathlessness, and dual bronchodilation would offer Stacy superior symptom control to monotherapy as her initial therapy14,17
- Stacy should be initiated with SPIOLTO® RESPIMAT® for superior symptom control from the start vs SPIRIVA®.14,17 In addition, the active delivery via a soft mist inhaler would be independent of Stacy's ability to inhale11,12
Dr. Miller's Simple Tools & Tips
- Infographics
- Content 1
- Inhalation Video
- Content 2
- Stand/Sit Exercise
-
- Patient Questionnaire
-
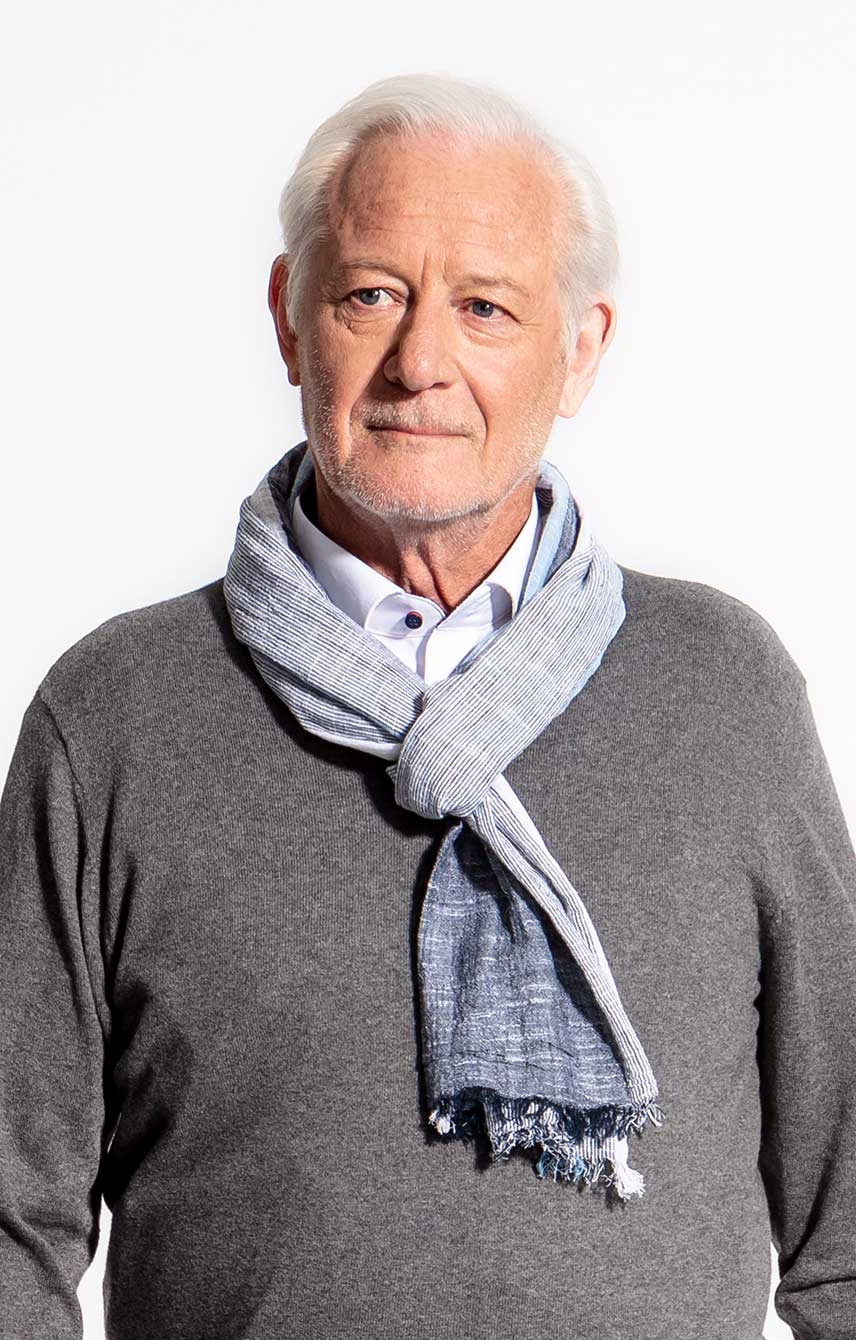
John, 53 years old
Background
- John is a landscape gardener. He was diagnosed with COPD 12 months ago
- John has severe breathlessness on exertion. He had a single exacerbation at diagnosis, which did not require hospitalisation. He has been finding it harder and harder to work due to the physical nature of his job, and over recent months sometimes hasn't been able to work at all. He used to be active, but now reduced his social and physical activities due to his symptoms
- John was initiated on LAMA monotherapy with SPIRIVA® HandiHaler® at diagnosis. His symptoms are not well controlled on monotherapy
Treatment considerations: initiation and next steps
- Up to 52% of COPD patients struggle to inhale from their device9
- ATS 2020 guidelines recommend LAMA/LABA as first-line treatment option in patients with dyspnoea or exercise intolerance4
- Monotherapy was not the optimal choice for John, because dual bronchodilation can provide superior symptom control from the time of diagnosis14,17
-
Switch to SPIOLTO® RESPIMAT® for:
- Active delivery of LAMA/LABA via a soft mist inhaler, independent of John's ability to inhale11,15
- An upgrade to LAMA/LABA, which offers superior symptom control over monotherapy14,17
- SPIOLTO® RESPIMAT® improves activity-related breathlessness and exercise endurance time,15,16 which can help John get back to work

Dr. Miller's Simple Tools & Tips
- Infographics
- Content 1
- Inhalation Video
- Content 2
- Stand/Sit Exercise
-
- Patient Questionnaire
-
James, 71 years old

Background
- Diagnosed with COPD 2.5 years ago
- James's symptoms include breathlessness on exertion. He had a minor exacerbation 2 years ago that did not require hospitalisation
- James's blood eosinophil count is 200 cells/μL
- He was initiated on LABA/inhaled corticosteroid at diagnosis
Treatment considerations: initiation and next steps
- LABA/inhaled corticosteroid was not the optimal choice for James. GOLD 2020 states that inhaled corticosteroid-containing therapies should be considered for some patients, with greatest likelihood of reducing exacerbations in patients with blood eosinophil count ≥300 cells /μL.3 James has a blood eosinophil of 200 cells/μL and a low risk of exacerbations
- Dual bronchodilation can provide superior patient outcomes vs LABA/ inhaled corticosteroid18,19 and the corticosteroid component does not offer benefit for patients like James – only the risks of pneumonia and long-term adverse events20
- Switch to LAMA/LABA therapy, which offers superior outcomes for patients like James, without the risks of an inhaled corticosteroid.18-20 In addition, the active delivery via a soft mist inhaler would be independent of James' ability to inhale11,12
- Upgrading to triple therapy would also improve symptom control with the LAMA/LABA, but the unnecessary long-term risks of inhaled corticosteroid would remain20
Dr. Miller's Simple Tools & Tips
- Infographics
- Content 1
- Inhalation Video
- Content 2
- Stand/Sit Exercise
-
- Patient Questionnaire
-
Julie, 76 years old
Background
- Diagnosed with COPD 3 years ago, when she was initiated on a LAMA for breathlessness (no exacerbations, blood eosinophil count 300 cells/µL)
- Following a mild exacerbation with continuous symptoms a year later, therapy was escalated to LAMA/LABA (plus influenza and pneumococcal vaccination), which controlled her symptoms without further exacerbation for 2 years
- Following two recent severe exacerbations, one of which required hospitalisation, Julie's blood eosinophil count was retested and found to be 400 cells/µL. Escalation of therapy is required
Treatment considerations: initiation and next steps
- Julie was initiated on LAMA monotherapy but after a year this was not sufficient for symptom control, necessitating escalation to dual bronchodilation.
- After a further 2 years on dual bronchodilation, Julie's high exacerbation risk3,4 and elevated blood eosinophil count3 called for the addition of an ICS to her LAMA/LABA therapy

Dr. Miller's Simple Tools & Tips
- Infographics
- Content 1
- Inhalation Video
- Content 2
- Stand/Sit Exercise
- Content 3
- Patient Questionnaire
-
Learn why Julie is one of the few patients that would benefit from ICS-containing therapies.
Learn moreFootnotes
- * Denotes patients with suboptimal peak inspiratory flow (sPIF), which is a measure of a patient's inspiratory effort, or ability to inhale. In a study, suboptimal PIF was defined as ≤60 L/min9,22
References
- Ferguson GT et al. NPJ Prim Care Respir Med. 2017;27(1):7.
- Buhl R et al. Eur Respir J. 2015;45:969-979.
- Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease; updated 2020. Available at: https://goldcopd.org/wpcontent/uploads/2019/11/GOLD-2020-REPORT-ver1.0wms.pdf
- American Thoracic Society. Pharmacologic Management of Chronic Obstructive Pulmonary Disease. An Official American Thoracic Society Clinical Practice Guideline. https://www.atsjournals.org/doi/pdf/10.1164/rccm.202003-0625ST
- Virchow JC et al. Respir Med. 2008;102(1):10-19.
- Newman SP. Eur Respir Rev. 2005;14:102-108.
- Mahler D. Ann Am Thorac Soc. 2017;14(7):1103-1107.
- Capstick TG, Clifton IJ. Expert Rev Respir Med. 2012;6(1):91-101.
- Loh CH et al. Ann Am Thorac Soc. 2017;14(8):1305-1311.
- Mahler D et al. Suboptimal PIFR associated with greater dyspnea in COPD [abstract]. In: Am J Respir Crit Care Med. 2019;199:A1132
- Anderson P et al. Int J Chron Obstruct Pulmon Dis. 2006;1(3):251-259.
- Zierenberg B. J Aerosol Med. 1999;12(suppl 1):S19-S24.
- Pitcairn G et al. J Aerosol Med. 2005;18(3):264-272.
- SPIOLTO® RESPIMAT® Summary of Product Characteristics, March 2020
- Maltais F et al. Eur Respir J. 2019;53(3).
- Troosters T et al. Am J Respir Crit Care Med. 2018;198(8):1021-1032 and supplementary material.
- Singh D et al. Respir Med. 2015;109(10):1312-1319 and supplementary information.
- Beeh KM et al. Int J Chron Obstruct Pulmon Dis. 2016;11:193-205.
- Wedzicha JA et al. N Engl J Med. 2016;374(23):2222-2234.
- Suissa S et al. Chest. 2019;155(6):1158-1165.
- Ghosh S et al. Int J Chron Obstruct Pulmon Dis. 2019;14:585-595.
- Sharma G et al. Chronic Obstr Pulm Dis. 2017;4(3):217–224.